Dr. Tom Oxley, CEO and co-founder of breakthrough brain-computer interface developer Synchron, discusses advances in minimally invasive neurointervention, medtech leadership, advice for device developers, and ethics at the bleeding edge of BCI technology.

Synchron co-founder and CEO Dr. Tom Oxley giving a TED Talk with an image of the Stentrode device displayed behind him. [Photo courtesy of Synchron]
What seems like a miracle today — a paralyzed patient regaining the ability to communicate with their family without open-brain surgery — may eventually seem obvious in retrospect.
It already does to Dr. Tom Oxley, the interventional neurologist who’s CEO and co-founder of brain-computer interface (BCI) developer Synchron.
Synchron’s Stentrode device is implanted inside a blood vessel in the brain to sense neural signals and relay them to another implant in the chest. Those signals are then translated into digital commands, allowing the patient to communicate electronically or control smart devices.
The FDA has given breakthrough device designation to the system, which Synchron is testing in six patients through its COMMAND trial. It’s the first FDA investigational device exemption (IDE) for any company assessing a permanently implanted BCI.
In an interview with Medical Design & Outsourcing, Oxley discussed Synchron’s mission and technology, device development challenges and ethical considerations of BCI innovation.

Synchron’s brain-computer interface (BCI) system uses the Stentrode brain implant to sense brain signals and relay them to a receiver implant in a patient’s chest. [Illustration courtesy of Synchron]
“Our vision is to build neurotechnology that solves the limitations of the human body. That’s a broad scope,” he said. “What we’re building is an interventional, blood-vessel-based product that can sense or stimulate in all areas of the brain. We think there’s a wide range of ways that can be applied, but our mission right now — the shorter-term mission — is to be the first to commercialize a brain-computer interface for motor impairment to help millions of people who are not able to access any treatment.”
Synchron is pushing toward FDA approval and commercialization before competitor Neuralink. Both companies are backed by billionaires: Jeff Bezos and Bill Gates are in Synchron’s corner, while Neuralink is owned by Elon Musk — who reportedly tried to invest in Synchron to hedge his bets.
Minimally invasive catheter delivery through the jugular vein and endothelialization of the nitinol Stentrode electrode stent are some of the biggest advantages for Synchron’s system over Neuralink, which plans to place its implant with open-brain surgery.
Oxley traces the idea back to his time in med school with co-founder Dr. Rahul Sharma, now director of structural interventions at Stanford Healthcare.
“He loved the heart, I love the brain,” Oxley said. “And I was always looking at what he was interested in like, ‘Why isn’t that happening in the brain yet?’”
Cardiologists now use advanced catheters for cardiac mapping and ablation and to place pacemakers, replacement valves and other implants.
“If that trajectory that happened in cardiology happened in the brain, imagine a world where you can have a procedure to have your brain mapped with electrophysiological data, and then some therapy [and] it’s fixed — no cutting of the skull,” he said. “… For me, that’s inevitably going to happen in the brain. And hopefully we can deliver.”
He sees opportunities for minimally invasive endovascular applications fo epilepsy and deep brain stimulation, and looks at the trajectory of interventional cardiology growth relative to cardiothoracic’s diminution and sees a universal trend that also applies to neurointervention.
“My dream was to bring neurointervention into the electronics era, and that includes sensing and stimulating. If all goes well, we will have created products that open up avenues to treatment of conditions that haven’t otherwise yet been possible,” Oxley said. ” … Neurointervention has a very bright future for neuroprosthetics, brain monitoring, brain mapping, ablation, and deep brain and brain stimulation. We have plans to do all of those.”
So why hasn’t anyone done what Synchron’s doing?
The key to the brain’s secret back door
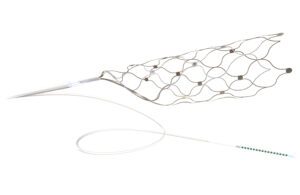
The Synchron Stentrode brain implant expands inside a blood vessel, placing its electrodes against the vessel wall to sense brain signals. [Image courtesy of Synchron]
How do you get into a patient’s brain without cutting a hole in their skull, which risks complications such as infection, stroke, seizures, brain swelling and nerve damage? The same way interventional neurologists can now mechanically remove clots blocking blood to the brains of stroke patients.
The recent explosion in neurovascular catheter technology opened the door for Synchron and created ranks of neurovascular physicians primed for new technologies, particularly elective procedures and devices.
At the same time, tech features from the likes of Amazon, Facebook, Google and Apple make it easier to communicate, shop and perform other daily tasks electronically.
“Hardware and software that let us live our lives with just the click of a button means that you can deliver high impact to your activities of daily living from a small amount of input into a digital device,” Oxley said.
But no one’s ever built a stent connecting to a lead before, presenting Synchron with a variety of novel challenges, including long-term safety. The catheter delivery challenge was a combination of three factors to be solved: the lead, the connection from the lead to the Stentrode implant, and the radial force of Stentrode itself.
“We had some necessarily stiff components of our system that needed to be offset with flexible components to achieve delivery. Delivery has been a huge challenge for us. … We’re still working through it now. We’re still making trade-offs,” he said.
Advice for other device developers

The Synchron BCI system includes the Stentrode implant, lead and chest implant (top left) that wirelessly transmits data to a decoder to translate the signals into digital commands. [Image courtesy of Synchron]
“You have to take it step by step,” Oxley said. “… Engineering perfection will stop you from getting to market quickly [and] learning. Maybe engineers don’t like and trust physicians that much, but give physicians a chance.”
One example: the advent of flow-diverting stents, with Medtronic’s Pipeline embolization device beating Stryker’s Surpass to market.
Stryker took longer “because they wanted to get the stiffness right. Pipeline came out really quick, but they had a very stiff device,” Oxley said. “You know what? The physicians could handle it. And the mechanical problem that hadn’t been solved pushed over to the physicians in the field, and they solved it.”
Leadership lessons
Oxley encourages speed from the corner office with a leadership style he described as “common sense, resilience, tenacity and sense of urgency.”
That leadership style has morphed into company values as Synchron has grown to around 70 employees. Oxley said he’s learned the importance of establishing and emphasizing those values to build a shared culture.
“They give people a framework to fall back on for decision-making when they’re not sure what to do,” he said.
At Synchron, common sense is an aversion to dogma in favor of pragmatism and meritocracy. “Every idea should be counted on its merits,” he said.
Sense of urgency — or bias for action — means empowering people to make a decision and keep moving. The company makes decisions with a personal, patient-first perspective: “Our quality policy is that our devices are good enough to be put in our loved ones,” he said.
Resilience is hard to build in a culture, and it’s something you often can’t teach. “People are either resilient or they’re not. But I certainly hire for that. I really respect it,” he said.
He also deploys the leadership concept of extreme ownership, which is “basically how able are you to absorb responsibility for things that are outside your obvious locus of control.”
“If you start to take on things that you’re not actually responsible for, but you think you can impact them, everyone’s circles are overlapping,” Oxley said. ” .. I have a bad reaction to people who have a problem absorbing responsibility, throwing blame or saying, ‘That wasn’t that wasn’t my thing to do.’ Especially in a startup, it really matters that you can reach out and try to own things that maybe you didn’t necessarily need to.”
Another leadership tenet is what they call “respectful candor,” or the ability to be upfront and open and speak one’s mind without being rude, pejorative or dismissive.
“If you trust and respect everyone, you can make a really direct comment. But you have to believe that the person you’re speaking to was doing their best, because when you start to think that they were not doing their best, then you can lose respect for people,” Oxley said.
Many of these values that Oxley’s prioritizes have come from his background in neurointervention, which he called “a brutal subspecialty.”
“You’re up in the middle of the night, and when complications happen in your intervention, it’s life-threatening and it’s at the end of your fingertips,” he said. “You have direct responsibility, and bad outcomes happen and then you have to deal with that.”
BCI ethics
There’s now a new responsibility to grapple with. Our thoughts are the only place where we are truly private, but minimally invasive BCI technology that can read brain signals might open a door that can’t be closed.
“I think the reason implantable brain-computer interfaces have captured the imagination of the public is because the technology points toward a potential of overcoming a limitation in the brain’s capacity to fully express itself,” Oxley said. “And that limitation is the control of the muscles of the body to provide verbal and nonverbal communication, which never quite captures what’s actually going on in your brain. We all have that feeling that you can never quite get across exactly what’s happening. That speaks to the limitation that we have. Our brains have much greater potential than what our bodies can live up to. And so that’s the principle by which — the idea that we are bypassing the human body as the mechanism of expression of the brain’s state.”
Asked how he grapples with potential harm from more advanced BCI technology in the wrong hands, Oxley said the benefits outweigh the risks, comparing it to the rise of artificial intelligence or the automobile.
“BCI is going to progress humanity. It’s going to relieve suffering and it’s going to improve capability in all directions. So then how do you protect against the nefarious things? It’s a serious question,” Oxley said. “I think relative to the other risks that are out there right now — for example, with AI where there’s zero regulation — we have very strict regulation with implantable devices going into the brain. There’s a whole cybersecurity section that we’re working on with the FDA. We have to be able to describe all of the possible flaws in our system. The FDA is doing an excellent job at regulating the safety of implantable medical devices, and we’re keeping up with that.”
Synchron’s currently only working in the motor control part of the brain, and it uses a different analytics process than might be able to measure brain signals for truthfulness or evasiveness, for example.
“We’re at the beginning of something brand new. … The brain is a huge place with lots of different areas to go and we’re going to have to depend on the FDA that when we start going into those areas of the brain where there is risk of [abuse,] there are absolute safeguards in place,” Oxley said.
For now, the potential benefits are clear and keep the Synchron team moving forward. Oxley described observing a patient as their system is activated and they regain control for the first time.
“They make a selection on the screen and their faces light up, they smile, they look at their wife. … it’s this most incredible moment,” Oxley said. “They have restored connection with their family. We feel like we’ve just given them back some element of agency.”