Learn about new and promising applications of energy-based medical systems and the challenges of developing them.
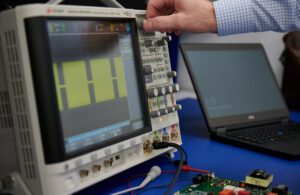
An engineer develops the pulsed waveform output for a PFA system. [Photo courtesy of Minnetronix Medical]
Daniel Friedrichs, Minnetronix Medical
While modern medicine is awash in high-tech electronics from large surgical robots to tiny implanted sensors, there are several applications where electrical energy is directly applied to a patient to ablate tissue, convey drugs, or achieve other clinical effects.
Given the obvious concerns with applying electricity to humans, developing these tools safely and effectively is crucial.
This article briefly reviews these applications of electrical energy in medicine and new opportunities to refine existing technology such as radiofrequency (RF) ablation or realize radical improvements using new energy modalities such as pulsed-field ablation (PFA).
Ablation
Use of energy to ablate diseased or disordered tissue can be affected using thermal means including RF, microwave and ultrasonic sources of heat.
RF is the most mature and prevalent technology, owing to its low cost, procedural simplicity, compatibility with minimally invasive techniques and well-understood performance. In RF ablation, high-frequency electrical current is conducted through an ablation target such as a tumor or nerve, causing heating and eventual cell death. The high frequency allows it to pass through tissue with minimal stimulation of muscle.
Modern RF ablation systems employ high-precision control systems which optimize ablation volume with minimal procedural time and can be tailored to specific clinical needs.
Pulsed-field ablation

RF ablation and PFA circuitry [Photo courtesy of Minnetronix Medical]
PFA is the use of high-strength electric fields to ablate cells through a non-thermal mechanism. Specifically, PFA degrades cellular membranes in an irreversible process leading to cell death.
RELATED: Pulsed-field ablation enables new precision cancer treatments
PFA differs from RF in that it is tissue-selective, non-thermal and conducive to pre-planning:
- Tissue-selective: Different tissue types have markedly different susceptibility to the electric fields employed in PFA, and this can permit tissue type-selective ablation. Cardiac electrophysiology applications are benefiting from this selectivity by utilizing PFA to ablate cardiomyocytes (which are highly susceptible to PFA) while avoiding unwanted collateral damage to the nearby smooth muscle of the esophagus (which is poorly susceptible to PFA). This selectivity may potentially provide significant reduction in morbidity for prostate and pancreatic cancer compared to RF or other treatments.
- Non-thermal: While thermal ablation causes tissue necrosis and a subsequent inflammatory response, PFA causes cell death through apoptosis, which is the natural mechanism of cellular clearance and is not inflammatory. Patients thus benefit from quicker post-procedure recovery.
- Conducive to pre-planning: Thermal ablation is difficult to pre-plan, as thermal properties of tissue — “heat sinks” from nearby blood vessels, “insulators” from nearby structures, and non-homogeneity of the ablation target — vary so significantly as to make pre-planning difficult or intractable. The electric field-mediated mechanism of PFA, however, is affected by a smaller, less variable set of parameters, allowing for meaningful pre-planning and control of energy delivery. Future applications of PFA are likely to include a patient-specific energy prescription derived from pre-procedural imaging and therapy simulation.
While PFA is an ablation tool, it also has a second act. By reducing the strength of the electric field, those same electric pulses can trigger a transient permeability in cell walls allowing injection of drugs, genes or other “cargo,” a technique variously called electroporation, electropermeabilization, or electrochemotherapy. By whatever name it goes, this is a macro-scale physical technique for modifying a cellular-scale biological process. Present clinical applications include conveying large-molecule drugs, DNA vaccines and delivery of customized gene therapies.
Use of electroporation to deliver such a drug turns the device into a combination product, triggering higher levels of regulatory concerns and scrutiny. In development of such a system, most important is a clear understanding of the interaction between the tissue and electric field and the boundary between reversible electroporation, irreversible electroporation (pulsed-field ablation) and thermal ablation.
RELATED: In vivo electroporation is an engineering solution for drug and gene delivery
Developing an energy-based system
For companies developing energy-based therapies, there are many considerations during early planning stages:
Translating experience with RF systems to PFA systems

An engineer makes adjustments to a RF ablation system used for comparison testing.[Photo courtesy of Minnetronix Medical]
Despite similar foundational architecture between RF and PFA, achieving the desired clinical outcomes is not trivial and can require many iterations.
That said, experience in RF design provides a solid foundation for developing of PFA systems. There are architectural similarities, as well as similarities in measuring clinical outputs that can be adapted. In setting out to develop a PFA system, having resources or partners that have extensive RF experience can help to limit pitfalls.
Design customization, avoiding platform entanglements
It is tempting to use a platform architecture for the capital hardware and focus development on the disposables or instruments. An off-the-shelf platform may give you speed to market for the first device, but will hinder expansion and generational improvements.
Being tied to a third-party platform can also entangle a developer in licensing agreements and hinders lifecycle planning. In a marketplace that will likely become as dynamic as any technology space in its early years, it behooves companies to develop their own capital systems for maximum flexibility expanding their portfolio.
Complete product lifecycle integration
It is surprising how many firms continue to plan development of complex systems like PFA programs in a piecemeal fashion. A typical system consists of several primary subsystems, and each of those consist of complex components and subassemblies.
A program of this magnitude needs to consider not just the immediate concerns of proof of concept to prototype, but how that prototype will translate through the process to commercialization.

Daniel Friedrichs [Photo courtesy of Minnetronix]
Daniel Friedrichs, Ph.D., leads development engineering efforts at Minnetronix Medical for commercialization of surgical energy devices including in vivo electroporation systems and other energy-based medical, surgical, and drug-delivery therapies. He is named on more than 35 patents and has worked with an extensive network of clients seeking to commercialize a wide array of technologies.