
[Photo from Pexels]
In 2020, researchers witnessed the emergence of post-acute sequelae of SARS-CoV-2 (PASC) — more commonly referred to as “long COVID.” Now, the notion of “long vax,” persistent and varying symptoms following COVID-19 vaccination, has come into focus, as Science has noted. This phenomenon, while not as widespread as long COVID, has concerned some in the medical community, potentially fueling vaccine hesitancy.
Still, serious adverse events stemming from COVID-19 vaccination are rare, typically occurring within six weeks of vaccination, as CDC notes. In addition, the majority of side effects following vaccination disappear within a few days. While such side effects are generally minor, a number of patients have had acute spells of dizziness post-vaccination, chronic hives and heart palpitations.
For those with long COVID and post-vaccination malaise, symptoms can include postural orthostatic tachycardia syndrome (POTS), a blood circulation disorder involving an increase in heart rate after standing. POTS can lead to symptoms such as dizziness or fainting.
Emerging concerns and implications of long vax
In 2021, Dr. Sujana Reddy of East Alabama Health published a case study on a patient who developed POTS after COVID-19 vaccination. She later learned of more than 250 people with similar health concerns. Reddy is working on a study documenting POTS cases, which includes 55 people who developed symptoms one to two weeks following vaccination.
In addition, research led by cardiologists at Cedars-Sinai Medical Center analyzed nearly 285,000 COVID-19 vaccination records and over 12,000 SARS-CoV-2 infection records from the Los Angeles area. Findings showed a 33% increase in POTS-related symptoms within 90 days following COVID-19 vaccination compared to the three months prior.
The overall rate of POTS occurrence, however, was lower than that following SARS-CoV-2 infection.The study also found that POTS-related diagnoses post-vaccination were higher than non-POTS-related diagnoses, with an odds ratio of 1.10. They found a more significant increase in cases of POTS among COVID-19 patients who were unvaccinated. These patients showed a post-infection risk that was 5.35 times higher after exposure to COVID-19 infection than after exposure to vaccination.
The Cedars-Sinai research was highlighted in Nature.
Linking POTS with vaccination and, especially, COVID-19 infection
Another study, published in Clinical and Experimental Emergency Medicine, also details the emergence of postural orthostatic tachycardia syndrome (POTS) in a subset of patients who had recovered from the acute infection of COVID-19.
Dr. Tae Chung, coauthor of the Clinical and Experimental Emergency Medicine paper, was originally hesitant to link POTS and COVID-19 vaccination but now finds the data convincing. Chung operates the POTS clinic at Johns Hopkins University. In the Science article, he continued to strongly promote vaccination, noting how vaccines protect against POTS, long COVID, and other symptoms.
Insights from Bristol University on the complex nature of Long COVID
Researchers at the University of Bristol have found that long COVID may not be caused primarily as a result of immune inflammatory reaction to COVID-19. In study published in eLife, they analyzed the immune responses of 63 patients who had been hospitalized with COVID-19 across a range of disease severities. Although they witnessed significant dysfunction in T-cell profiles in severe cases at three months, indicating persistent inflammation, this resolved over time. By 12 months, both immune profiles and inflammatory levels were similar across patients regardless of disease severity. Ultimately, they found no clear link between long COVID symptoms and immune inflammatory responses. The researchers did note an increase in T-cells targeting Cytomegalovirus (CMV), suggesting that prolonged T-cell activation might instead be driven by “bystander” mechanisms unrelated to SARS-CoV-2.
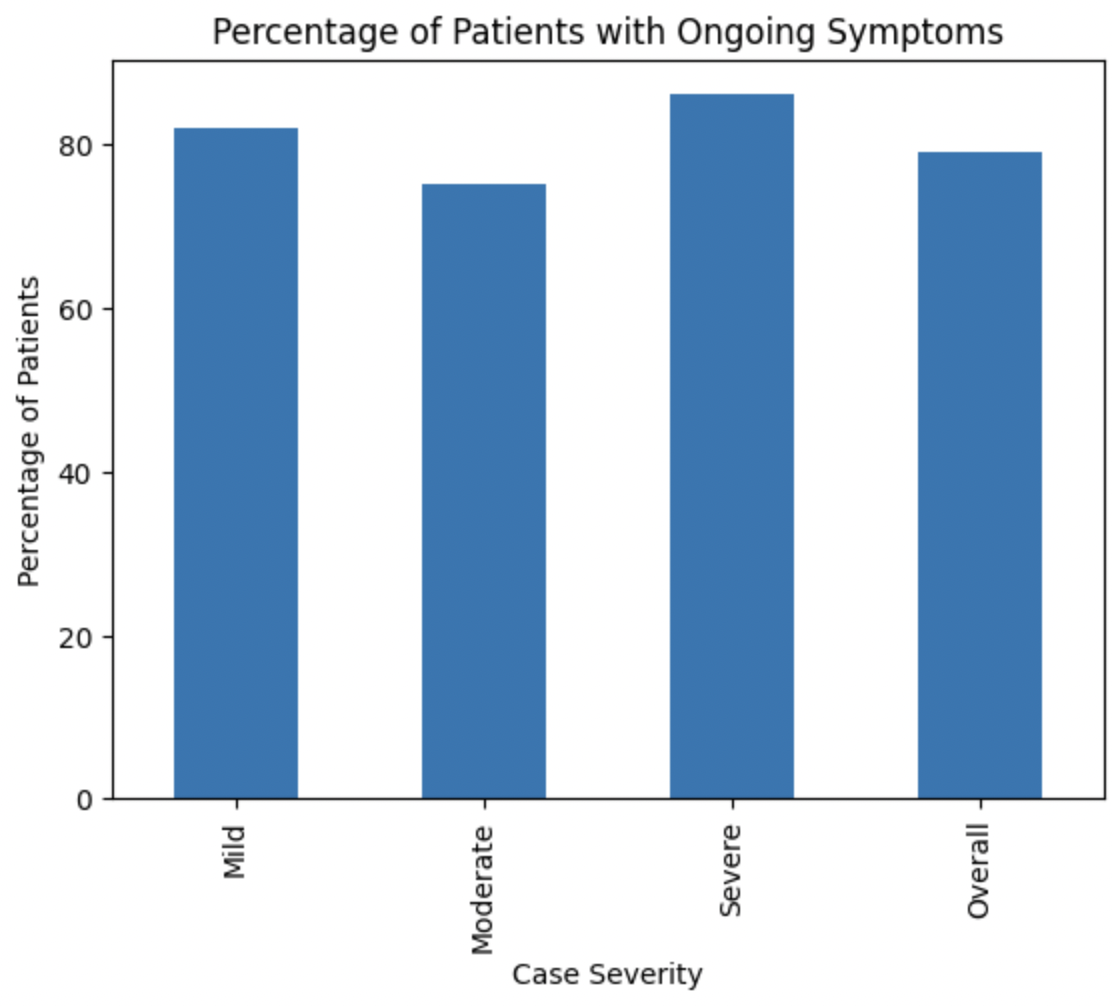
- Bar chart showing the proportion of COVID-19 patients with long-term symptoms, categorized by disease severity. University of Bristol researchers collected the data from 63 patients hospitalized with COVID-19. They tested for immune responses at the 3-month, 8-month and 12-month marks post hospital admission. A total of 82%, 75% and 86% of patients with mild, moderate and severe disease severity, respectively, reported at least one lingering symptom, with breathlessness and excessive fatigue most commonly reported.