
The body of the Hamilton Medical proximal flow sensor consists of two molded halves composed of medical-grade plastic. Between the two halves, a ring-shaped insert holds a delicate membrane with a variable orifice that detects changes in air direction and flow within the patient airway, transmitting inhalation/exhalation inputs to the ventilator digital control through two small tubes linked to the ports at center right. These inputs are used to minutely regulate air pressure and flow in real time. [Photo courtesy of Hamilton Medical]
The disposable sensor monitors ventilation of critically ill patients with high precision.
Didier Perret, Emerson
Hamilton Medical (Bonaduz, Switzerland) produces intelligent ventilation solutions for intensive-care units and critical-care transports. To meet the exploding demand for ventilators during the COVID-19 pandemic, Hamilton Medical established a new ventilator production site in Reno, Nevada, with the support of a local team from General Motors.
In four months, the facility moved from bare floor to full production, delivering the first of thousands of Hamilton-T1 ventilators purchased under contract by the U.S. Department of Health and Human Services (DHHS) in September 2020.
Mass producing proximal flow sensors
Since 1983, the proximal flow sensor has been the centerpiece of all Hamilton Medical ventilators. It provides valuable data directly from the patient’s airway opening. The sensor must be able to detect even tiny pressure changes that signal a patient’s attempts to breathe naturally, adjusting to the patient’s own inhalation process to comfortably support it with the required volume of oxygenated air.
Successfully mass-producing highly engineered and extremely precise flow sensors from disposable components was not simple; it posed significant design, assembly and cost challenges for Hamilton Medical. Fortunately, the company had already invested in years of design and development efforts in Switzerland, collaborating with Emerson and local machine builders to create and validate automated systems for assembling all-plastic flow sensors using Branson ultrasonic welding technology. Ultrasonic welding combines high-frequency vibration and compressive force to create frictional heating and targeted melting at the interface of mating thermoplastic parts, enabling them to join permanently. The process is well suited to flow-sensor assembly, since it virtually eliminates risk of heat, mechanical stress, or contamination to the sensor’s fragile membrane.
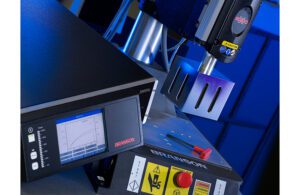
The Branson 2000Xc ultrasonic welder [Photo courtesy of Emerson]
The fully automated flow-sensor assembly system was built by Switzerland-based Imperia Systems under the supervision of Hamilton, with Emerson providing medical-production-ready Branson 2000Xc ultrasonic welders, weld tooling, and technical and integration support to the fast-track assembly project. Following delivery, the system underwent successful IQ/OQ/PQ (installation, operational and performance qualification) in time for the September 2020 production launch.
During operation, the assembly system robot picks and positions the three sensor components atop the lower weld tool. First comes the lower half, into which is inserted the flap containing the membrane. After the robot validates proper ring-membrane position, the upper half is placed on top. Then, the actuator of the welder descends, compressing the upper weld tooling onto the sensor components. Compressive force actuates the ultrasonic weld, which is completed in less than one second.
As the ultrasonic weld is made, the digital controls in the welder monitor all weld parameters in real time and save a complete weld data record for each part. Medical-ready Branson welders are equipped with data security features including hierarchical password protection and high-grade data encryption. They support compliance with leading global manufacturing standards including ISO 13485, as well as medical device production and part traceability requirements in the European Union’s Medical Device Regulation and the FDA’s 21 CFR Part 11 regulations.
How ventilators work
Mechanical ventilators like the Hamilton-T1 provide respiratory support to the lungs of patients who are unable to breathe sufficiently by themselves due to injury or respiratory disease.
Following intubation — the insertion of an endotracheal tube into a patient’s trachea — ventilators offer multiple modes for safely providing the lungs with sufficient oxygen and removing carbon dioxide. Modes are selected based on the patient’s remaining respiratory capacity and range from fully automated to supportive (e.g., triggered by the patient’s own efforts to breathe).
And especially with the help of intelligent digital controls, automating the human respiratory process involves great precision and complexity. Ventilators may deliver a high-oxygen mixture at a carefully managed pressure, breath volume, respiration rate, humidity level and temperature. Hamilton Medical ventilators follow the principle of intermittent positive pressure ventilation (IPPV). Gas with a defined oxygen concentration moves under positive pressure to the lungs, passing through bronchial tubes into tiny individual air sacs (alveoli). In the alveoli, the gas exchange takes place: Oxygen is exchanged with carbon dioxide at the red blood cells. During expiration, the ventilator’s exhalation valve opens to relieve the pressure, and the gas enriched with carbon dioxide can escape through the alveoli from the lungs and out of the body.

When the inspiratory valve opens, the positive pressure (airway opening pressure, or PAO) drives air into the circuit, filling the circuit and inflating the lung until the set inspiratory pressure is achieved. This provides the required ventilation of the lungs, pushes O2 and retracts carbon oxide through the alveolar membrane to the bloodstream. Then, the expiratory valve opens, air pressure is released from the circuit, and the lung naturally deflates as carbon dioxide and other gases are vented out. [Illustration courtesy of Emerson]
A circuit of two tubes, attached to the ventilator and the patient’s airway, constitutes the breathing circuit. The two tubes meet at a Y-piece, with the inhalation tube and valve on one branch, the exhalation branch and valve on the other. At the Y-piece the breathing gas passes through the proximal flow sensor, moving to and from the patient airway.
This process itself is relatively simple — alternating cycles of higher pressure for inhalation and pressure release for exhalation. The complexity stems from the precision needed to replicate fine adjustments that a patient’s brain would otherwise make to regulate the breathing process. This calls for accurate real-time control of myriad factors: mixture, flow rate, pressure and even the timing of each breath.

Didier Perret [Photo courtesy of Emerson]
Didier Perret is the medical business development manager, Branson Welding and Assembly at Emerson. He has a degree in mechanical engineering from Technicum La Chaux-de-Fonds in Switzerland. Perret has worked for Emerson since 2000 and has extensive experience in automation, production, product design and plastics assembly technologies.
The opinions expressed in this post are the author’s only and do not necessarily reflect those of MedicalDesignandOutsourcing.com or its employees.