
The Synchron brain-computer interface system relays signals from the brain to a device in the chest, then translates the signals into action on a computer. [Image courtesy of Synchron]
Officials at Synchron, the developer of the catheter-delivered Stentrode brain-computer interface (BCI) implant, believe they’re the only BCI company tapping into blood vessels to capture signals from the brain.
They say they’ve already enabled a small group of paralyzed ALS patients to control a computer with their minds, and hope there will be more applications of their technology.
Shortly after the New York-based company released new results of a safety study for its implant, Synchron Director of Neuroscience Peter Yoo spoke with Medical Design & Outsourcing about the Stentrode implant and how catheter delivery could make BCI technology simpler, safer and more accessible than the leading alternative: open-brain surgery.

Peter Yoo is the director of neuroscience at Synchron [Photo courtesy of Synchron]
“The novel approach of the catheter delivery increases the number of physicians who can deliver our devices compared to a very specialized type of surgery,” Yoo said in an interview. “The techniques that we use are standard angiography procedures and other neurointerventional techniques performed by stroke doctors. We’re hoping that it’ll help with the proliferation of the technology and access to the technology, that it can be cheaper and more available for the patients who are in need.”
This conversation has been edited for space and clarity.
MDO: How did BCI technology get to where it is today?
Yoo: BCI has been on a bit of a journey. It’s been in the making for a few decades now, but it hasn’t quite translated into the real-life patient setting yet. It’s largely been an engineering problem because people need to pave the way of getting into the brain or getting inside the skull to record these high-fidelity signals. … The other side of the technology, the user experience and UI and the software and the commercialization side of the product, has largely been worked on recently. It’s moving quite quickly now, this space. The initial focus was largely on trying to regain physical mobility — exoskeletal controls and robotic limbs — but most of the space has moved on to controlling digital devices. Smart devices are essentially ubiquitous. We’re trying to catch all of these timely aspects to create our first commercial BCI product that can make an impact in patients’ homes. So that’s what Synchron is really focusing on, not just an engineering challenge, but a commercial product challenge as well, trying to make a BCI that’s actually usable at home without needing a Ph.D. neuroscientist to set everything up.
MDO: Was Synchron focused on catheter delivery from the start?
Yoo: Neurointervention is a relatively newer field, but it is now an established field where people are routinely going into the brain through the vasculature without needing to perform a craniotomy or open brain surgery [for] intracranial stenting to treat some conditions, for clot retrieval, coiling and those sorts of stuff. Very similar to the cardiac space, that’s how we always used to start. It was mechanical problem solving, but then they quickly transitioned into cardiac EP (electrophysiology), putting electronics and devices onto those mechanical devices. So that’s the route that appeared obvious to us, obvious to Tom (co-founder and CEO Dr. Thomas Oxley), because he was a neurologist working in the stroke space. We decided to mount electronics onto the stents that give us natural access into the brain without needing to open up the skull. Fortuitously, the human brain and many other mammals have this natural venous pathway that goes into the brain. … We’re exploring those pathways to get into the brain using standard, routinely performed techniques through angiography.
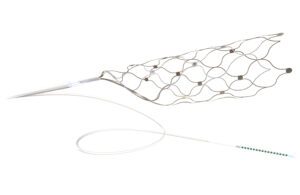
The Synchron Stentrode brain implant expands inside a blood vessel, placing its electrodes against the vessel wall to sense brain signals. [Image courtesy of Synchron]
MDO: Were there any obstacles presented by catheter delivery?
Yoo: The main challenge was there was essentially a lack of chronic data of leaving a device inside the blood vessel permanently. There is one routine case now: treating intracranial idiopathic hypertension [where] for an unknown reason, intracranial pressure builds up. People have been putting a stent into the transverse sinus — which is the sinus that runs along back of the head sideways — permanently placing stents there with less than a 2% major complication rate. But that’s the only chronic-stenting-inside-the-brain data that’s available. So we had to do a lot of work in the background, benchtop testing and some large-animal testing to make sure that leaving a permanent device with the lead inside the blood vessel doesn’t cause thrombosis or any other health risks.
MDO: Why does it need to be permanent?
Yoo: The stent gets incorporated into the brain and that helps with a few things. That improves the isolation of the electrodes so it doesn’t come in contact with the blood and other things that are conductive. The electrodes inside the blood vessel secure the device in position and improves our ability to record the signal, so that increases stability and fidelity. … We are researching the safety profile of removing the device … but currently it’s a permanent device.
MDO: What were the big engineering challenges your team had to overcome?
Yoo: Full disclosure: Manufacturing and hardware design is not my particular domain of expertise. But we had to create a lot of the processes from scratch. Mounting electronics onto stents that are going to be permanently implanted didn’t exist prior to us. We started off manually making them, now we’re printing them. All of those processes and methods had to be created from scratch, leaning on a lot of other manufacturing practices and know-how. And we had to solve the problem of once you make those recording heads, the sensors, then how do we connect those into blood vessels and connect it into some transmitting units. All of those transition zones and coming up with electronics to wirelessly transmit the data out of the body was also a problem and a challenge. The tortuosity of the blood vessels means that the device had to be flexible, yet firm enough so that you can push the device into the brain through those tortuosities. Getting those sweet spots right was definitely a challenge for our mechanical team.
MDO: How is this device implanted?
Yoo: We do a direct internal jugular vein (IJV) puncture — we don’t do a cut-down — to access the blood vessel. From that point for most individuals, there is a pathway through the IJV that goes off the sigmoid — which is this coily, roundy bit — into the transverse sinus and then into our target vessel, which is the superior central sinus. This nice pathway goes all the way from the IJV to the target blood vessel location at the top of the brain. Once you’ve delivered the device through a series of catheters and unsheath all the catheters, you have the lead of the device sticking out from the IJV. From that point, we do a standard tunneling procedure — which is often done in the cardiac EP space for implantable pulse generators — to tunnel the lead under the skin into a small chest pocket and place the telemetry unit inside the chest pocket. Essentially, the wire goes under the skin, comes out of a pocket, we plug it in. Then we put the rest of it inside the chest pocket. Everything’s completely inside the body. That’s obviously very good for infection control. Some of the other devices have transcutaneous connections, which means that it’s not fully implanted. With our device, we really made careful designs to make sure that the implantables are fully implanted and the data transmission is wireless, because we’re getting to the brain and we’re very proactive about controlling infection.

The Synchron BCI system relays data from the brain to a transmitter in the chest that wirelessly beams the data to another device outside of the patient. [Image courtesy of Synchron]
MDO: And then that wireless data connects to a smartphone or a computer?
Yoo: Our current iteration of the device is transmitting the raw data from the implantable through an RF link. Because it’s a custom communication protocol, it goes into a little intermediary box so we can sample the signal, and then that goes straight into a commercial laptop where it was running our algorithms so we can translate the incoming signals into digital outputs so the patient can use generic, consumer-grade software and hardware at home without needing a big box or specialized equipment.
MDO: How else might this technology be used?
Yoo: Essentially, we’re trying to sense. We’re starting out with brain-computer interfaces as an application, we’re listening to the brain and that can be either used to control digital devices as we’re doing now, or it can be used to acutely diagnose some conditions like epilepsy. … Also, we can send information back into the brain — that’s stimulation, we’ve published some previous work on that — which means we can provide therapy through stimulation of the brain as this field has been doing for a long time with deep brain stimulation. That can treat a variety of conditions potentially.
MDO: What are those conditions?
Yoo: All the blood vessels that proliferate throughout the brain, theoretically we can get to those places, given that they are not too small. There will be some lower limit of tiny venules or tiny arterials that with current technology, it would be difficult to get to, but there are many, many, many millions of small vessels that you could potentially reach. Currently, the way that deep brain stimulation reaches those areas is by performing a craniotomy and putting a rod in. Obviously, that has its own risks, but when targeted correctly and you stimulate specific parts of the deep brain areas that have been studied for decades, you can cause really good symptom relief effects. We would be doing exactly the same thing, except we’ll be reaching those areas through the blood vessels and stimulating from within the blood vessel, which means that we don’t need to come in contact with the brain directly, which has its own set of advantages in terms of immune responses. It’s nice to just leave the brain alone and talk to it and speak to it from a distance.
MDO: Are there any advances in technology that you’re looking for that will open up some of those smaller paths to the brain, like miniaturization of catheters or downsizing of the electrodes?
Yoo: That’s just continued, ongoing work of the R&D team, to continue to miniaturize and improve access methods to get to those smaller places. That’s ongoing work that’s done at Synchron.