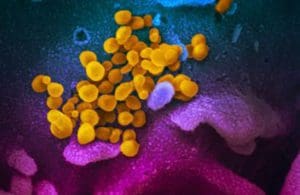
A scanning electron microscope image shows SARS-CoV-2 (yellow). Credit: NIAID-RML
It may be too soon to know how often the omicron variant is associated with so-called long-COVID, but research from the Leavitt Partners’ COVID-19 Patient Recovery Alliance confirms that vaccination protects against the condition.
Those who received at least one authorized COVID-19 vaccine dose before diagnosis were between seven and 10 times less likely to report two or more long-COVID-19 symptoms, according to the preprint study conducted before the surge of the delta variant.
Those who received a vaccine four weeks after diagnosis were four to six times less likely to develop the condition.
There are limits to how well researchers understand the condition given the fuzziness of the definition of long-COVID and the continual emergence of SARS-CoV-2 variants, said Michael A. Simon, principal data scientist at Arcadia Healthcare Solutions, who was involved in the preprint research.
“There’s a lot of information going around and a lot of different kinds of studies,” Simon said. “It’s a little harder to have some cut-and-dried answers.”

Michael Simon
For one thing, it can be difficult to come up with a universal definition of long-COVID, or post-acute sequelae SARS-CoV-2 infection (PASC).
In their observational study involving the medical history of 240,648 COVID-19-infected individuals, the COVID-19 Patient Recovery Alliance found that long-COVID is a common phenomenon based on data from the U.S. healthcare system that excluded children. Although symptoms such as fatigue, loss of sense of smell, shortness of breath, vomiting, headaches and so forth are found in the broader population, they are considerably more common in those with prior COVID-19 infections. And those with prior COVID infections were likely to have a constellation of symptoms rather than a single complaint.
A study recently published in The Lancet reached similar conclusions based on data from a self-reporting app involving 1.266 million people. That study found that having two vaccine doses cut the chances of having symptoms for 28 days or more in half.
“This is an uptick in individuals who are reporting multiple long-term symptoms that have been emblematic of their COVID experience,” Simon said.
Separate studies in Cell and Nature Communications identified a handful of factors that appear to increase the risk of long-COVID.
The NIH has committed to spending $1.14 billion to investigate long COVID,” which it describes as a “public health priority.”
The Brookings Institution recently concluded long-COVID was a partial explanation of the U.S. labor shortage, accounting for approximately 15% of unfilled jobs.
It is too early to know if the omicron variant is likely associated with a reduced risk of long-COVID than earlier variants.
The omicron variant began to drive a surge in infections in late December in much of the world.
“If you look at the timespan you need to understand long-COVID, we will only have the data in hand to start thinking about that in the next few weeks,” Simon said.
A slew of questions related to long-COVID remain unanswered, such as the possibility of the novel coronavirus leading to the onset of chronic conditions, including possible neurological symptoms or worsening of existing neurological issues.
“There are a lot of aspects there that we haven’t had enough of a chance to investigate and that are another level beyond whether individuals are still having fevers or are tired and so on,” Simon said.
Arcadia plans on conducting further research on long-COVID based on feedback from the COVID-19 Patient Recovery Alliance and other researchers. “We’re going to bring in some more data attributes such as the onset of other chronic conditions,” Simon said.
The company also plans to look at data before and during the delta wave. “I don’t think we’ll have omicron data yet,” he said, but the company plans on analyzing such data when it becomes available.
Arcadia plans on analyzing the pandemic’s impact on preventive care. “We asked hypothetically in early 2021 what the negative repercussions of the delay of preventive care would be,” Simon said. Now, those repercussions are beginning to become apparent.
“It’s not just those who are suffering from COVID or long-COVID, but those who made choices during the pandemic who need additional health care,” Simon concluded.