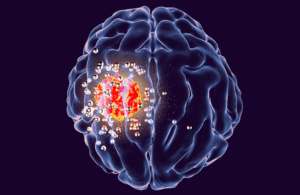
Researchers think a wireless implant to treat brain tumors could eliminate hospital visits for cancer treatment. [Image courtesy of Stanford Medicine]
Researchers at Stanford Medicine have developed a small wireless device that could wirelessly remove deadly brain tumors.
According to the researchers, brain tumors are some of the most deadly and difficult-to-treat cancers. Glioblastoma, an aggressive form of brain tumor, kills more than 10,000 Americans a year.
Treating brain tumors typically involves open-skull surgery to remove as much of the tumor as possible, followed by chemotherapy or radiation. Each treatment option comes with serious side effects and numerous hospital visits.
Stanford Medicine researchers believe they can painlessly and wirelessly, without anesthesia, treat the tumors from a patient’s home.
The researchers developed a small, wireless implant that is remotely activated to heat up nanoparticles injected into the tumor to gradually kill cancerous cells. In mice with brain tumors, 15 minutes of treatment over 15 days while the animal continued their normal routines increased survival times.
“The nanoparticles help us target the treatment to only the tumor, so the side effects will be relatively less compared with chemotherapy and radiation,” said Hamed Arami, PhD, co-lead author of the paper, a former postdoctoral fellow at Stanford Medicine who is now at Arizona State University.
Photothermal treatment of brain tumors has been used before, but could only be performed during surgical procedures when the brain tumor was exposed to the light source. The Stanford Medicine researchers hope to develop a system that does not require baring the brain.
The Stanford Medicine research team, in collaboration with Stanford University electrical engineering professor Ada Poon, developed a system that can generate heat precisely at the site of the tumors to kill them. The wirelessly-powered device is implanted between the skin and the skull. Specially designed gold nanoparticles are injected into the tumor through a tiny hole in the skull.
When the device is powered on, it emits infrared light that can penetrate brain tissue to activate the nanoparticles, which increase in temperature by up to 5º Celsius, enough to kill the cancer cells over repeated treatments without damaging the surrounding brain tissue.
Researchers can target tumors of different sizes and brain locations by adjusting the power and wavelength of light. The structure and dosage of the nanoparticles are calibrated to generate just the right amount of heat, according to the researchers.
So far, the researchers have tested their device in mice that had received human-derived brain tumors and the mice appeared to be undisturbed. They also showed that the injected nanoparticles stayed at the tumor site and did not endanger surrounding tissues.
“We think this short amount of heating, which is in the clinically acceptable range, is not affecting normal activities,” Arami said.
Treated mice lived “significantly longer” than the untreated mice – some with doubled or tripled survival times on average. However, the researchers cautioned that it is difficult to extrapolate survival benefits across species with such different lifespans. When the new treatment was combined with chemotherapy, the mice lived even longer.
“Glioblastoma patients don’t often live more than two to three years after diagnosis because you can’t get rid of every part of the tumor, and the tumor can become drug-resistant or radiation-resistant,” Arami said. “The goal is to combine this with other treatments to extend survival.”
The researchers hope that their device, when adapted for human use, could be for in-home treatment in addition to surgery, chemotherapy or radiation to eliminate the burden of hospital visits.
“With the rapid progress in the field of device development, I think that, in the next five years, we’ll be able to develop devices that can generate even more optical powers for deeper tumors,” Arami said.
Stanford Medicine’s research was published in the journal Nature Nanotechnology.