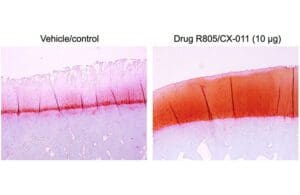
The left image depicts osteoarthritic cartilage damage in animal studies without any treatment, while the right image reveals articular cartilage regeneration following a knee injection of the novel drug R805/CX-011. [Image: Evseenko Lab/USC Stem Cell]
Researchers at the Keck School of Medicine at the University of Southern California (USC) have discovered a drug compound, R805/CX-011, with the potential to alleviate the painful hyperinflammation from osteoarthritis. The findings concerning the prospective osteoarthritis treatment breakthrough, published in Science Translational Medicine, showed positive effects in animal models and could pave the way for human trials.
We recently had the opportunity to speak with Dr. Denis Evseenko, a professor of orthopedic surgery, stem cell research, and regenerative medicine at the Keck School of Medicine, about the research. In the Q&A, Dr. Evseenko discusses the potential impact of R805/CX-011 on osteoarthritis patients, the drug compound’s mechanism of action, the role of the GP130 receptor in osteoarthritis, and the upcoming clinical trials of R805/CX-011 for the potential osteoarthritis treatment breakthrough. He also talks about the potential benefits of this breakthrough for patients and plans to explore its efficacy in other medical conditions such as pulmonary fibrosis and bone loss resulting from chronic obesity.
The responses have been lightly edited.
Can you talk about the potential impact of R805/CX-011 to be an osteoarthritis treatment breakthrough?
Evseenko: Osteoarthritis has no real solution. There’s approximately 500 million people worldwide with osteoarthritis with pretty much no options except for total joint replacement. If you look at the pipeline, it’s pretty much empty. There are a couple of drugs in phase 1 in development, but there are almost no candidates in the clinic for this disease and one of them is at USC. So I think that’s important.
Can you tell us more about the drug compound R805/CX-011 and its mechanism of action?
Evseenko: In spontaneous osteoarthritis, which often occurs with aging, there is activation of chronic mechanisms, particularly signaling through the interleukin-6 receptor, GP130. This receptor is ubiquitously expressed and crucial for connective tissue, as it controls many immune reactions. Over the past five years, it has been demonstrated that GP130 can drive multiple regenerative outputs. However, in disease, the receptor is engaged in a pathological manner, switching from transmitting regenerative signals to promoting degenerative ones. As a result, GP130 is described as a stress sensor.
Under stress, cells like chondrocytes, which produce a complex matrix and utilize macromolecules like glucose and amino acids, struggle to maintain anabolism. This leads to a catabolic state and degenerative outcomes driven by GP130. R805, the compound in question, does not merely inhibit the receptor; it pushes GP130 into a more anabolic, regenerative mode, biasing it towards signaling outputs typically found in stem cells. The target is GP130, and the mechanism of action biases the receptor’s activation signals to only promote anabolic outputs such as cell proliferation, cell survival, and matrix protein production in chondrocytes.
Another critical cell type affected by R805 is residential macrophages, which constantly communicate with cells in the joint. When cartilage degenerates, it releases molecules that imitate the processes seen in infectious diseases. Macrophages sense these molecules and activate inflammatory reactions to fix the problem, stimulating new blood vessels and removing unhealthy cells. They use GP130 for this purpose, and R805 helps drive the receptor towards a regenerative mode.
Our studies in animal models demonstrated that the drug compound can disrupt the receptor’s over-activation of inflammation while still managing pain and stiffness. We observed a profound effect on joint pain, structure, and function.
What role does the GP130 receptor play in osteoarthritis, and how does R805/CX-011 affect it?
Evseenko: GP130 recruits white blood cells to launch an offensive against infections. However, it can also summon these cells in response to broken pieces of cartilage from our joints, resulting in hyper-inflammation in the joints, known as osteoarthritis. Our research suggests that blocking just one of GP130’s many signaling cascades with R805/CX-011 or genetic modification may prevent the hyper-inflammatory response that characterizes osteoarthritis. We also observed signs in animal models that the interventions could lead to tissue regeneration and healing.
Can you share more information about the upcoming clinical trials of R805/CX-011 for osteoarthritis treatment?
Evseenko: This year, we’ll launch a combined safety and preliminary efficacy clinical trial (Phases 1 and 2A) of R805/CX-011 for the treatment of osteoarthritis in patients in collaboration with the start-up Carthronix. We have received more than $5 million from the Department of Defense to fund this research, which will test R805/CX-011 knee injections in up to 70 patients.
Could you say more on R805/CX-011’s potential to be an osteoarthritis treatment breakthrough?
Evseenko: R805/CX-011 injections may offer a less expensive and less invasive option that could be administered several times a year in an outpatient clinic. It has the potential to delay or even reduce the need for joint replacement surgery, the only existing FDA-approved therapy for osteoarthritis. Furthermore, this drug could help prevent opioid addiction, which affects an estimated 1 million osteoarthritis patients in the U.S.
The primary outcome measure will be the level of pain experienced. Chronic osteoarthritic pain is quite different from acute pain, which can be alleviated by NSAIDs or other treatments. This type of pain is largely unresponsive to treatment, leading people to undergo joint replacements or resort to opioids as their only option for relief. This chronic pain is self-sustaining and is associated with changes in dorsal ganglion neurons. The GP130 receptor, the target for R805, has been shown to critically regulate pain levels and pain thresholds. This is connected to nociceptive neurons in osteoarthritis, leading to a distinct, pathological pain sensation. The disease lowers the threshold for sensing pain, so it is essential to recognize that osteoarthritis in humans is primarily a pain disease.
In the past five years, at least three major pharmaceutical companies have halted phase 2 trials due to insufficient pain relief outcomes. These trials were stopped because the drugs did not produce the desired results in the pain arena. This is one of the reasons we wanted to conduct a comprehensive large animal study that closely mimics human trials. Pharmacological mechanisms and cell biology are crucial, but if the desired outcomes are not achieved, it is challenging to succeed in human trials. This is a critical point, as many people continue to struggle with osteoarthritis pain.
Are there plans to explore the efficacy of R805/CX-011 for other medical conditions?
Evseenko: Yes, we plan to investigate the potential of R805/CX-011 for stimulating tissue regeneration in a broad range of other medical conditions, including pulmonary fibrosis and bone loss resulting from chronic obesity.