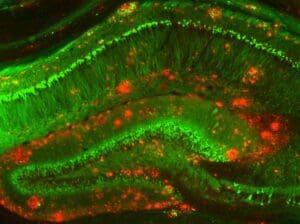
Mouse model of Alzheimer’s disease [Image courtesy of NIH]
The recent announcement by Eisai/Biogen of the positive outcome of the CLARITY study of lecanemab — an antibody that preferentially targets soluble toxic beta-amyloid aggregates (protofibrils and oligomers) — supports the decades of research, overwhelming genetic data, and basic understanding that beta-amyloid is a bad actor in the Alzheimer’s disease process. It is also much-welcomed news for patients and their families who have long waited for a treatment that can slow this previously inexorable disease.
Cognition Therapeutics is pursuing a novel approach focusing on the same target – oligomeric amyloid beta. However, instead of attempting to remove amyloid from the brain, our oral small molecule (CT1812) is designed to modulate a key cellular receptor (sigma-2) that prevents oligomers from binding to neurons and thus blocks their synaptotoxic effects. Based on findings presented by Eisai at the Clinical Trials in Alzheimer’s Disease (CTAD) in December 2022 and published in the New England Journal of Medicine, we believe this new mechanism of action is fundamentally distinct and complementary to that of anti-amyloid antibody-based immunotherapy. As further validation, the National Institutes of Aging branch of the NIH has awarded us multiple grants to evaluate this approach in the clinic.
Eisai, Biogen and BioArctic are to be applauded for doggedly following the science and successfully completing the CLARITY trial with what is believed to be a clear and unambiguous signal. However, several commentators have pointed out that while the clinical benefit is significant (CDR-SB treatment difference of 0.45 versus placebo, corresponding to a 27% slowing), it leaves much room for improvement and further slowing of the rate of disease progression.
Several reasons why disease progression continues despite “amyloid normalization” have been proposed:
- Despite removing amyloid plaque and fibrils measurable by PET imaging, toxic oligomers remain, directly damaging sensitive brain synapses and driving neuroinflammation.
- Alternate amyloid-mediated mechanisms of neuronal injury may be acting upstream of tau-driven pathology.
- Because it is downstream of amyloid beta, once initiated, tau pathology progresses despite lowering amyloid load.
The sigma-2 receptor complex is believed to be a central cellular signaling node involved in regulating damage response mechanisms, which are triggered in Alzheimer’s and other neurodegenerative diseases. Such mechanisms involve the regulation of cholesterol biosynthesis, vesicle trafficking and other key processes. While a fuller understanding of the molecular mechanisms involving the sigma-2 receptor complex remains to be elucidated, evidence suggests that targeting this receptor complex may provide therapeutic benefit to a wide range of age-related degenerative diseases and disorders.
Indeed, extensive pre-clinical data have shown that modulating sigma-2 to displace amyloid oligomer binding can reduce synaptic toxicity. It is also implicated in processes such as autophagy and neuroinflammation, which are known to be disrupted in Alzheimer’s and other neurodegenerative diseases.
Early-stage clinical studies with the oral, small molecule called CT1812 support our belief that it may alter these processes in Alzheimer’s patients as indicated by proteomic analysis of specific biomarkers predictive of synaptic injury and neuroinflammation. In initial clinical studies, CT1812 has been well tolerated and shown a trend towards cognitive benefit and evidence of slowing brain atrophy. Larger randomized controlled trials are now ongoing for CT1812 in Alzheimer’s disease and lesser-known dementia with Lewy bodies, with the support of $170M in competitive grant funding from the NIH.
Elsewhere in the industry, we are seeing a variety of approaches that aim to address the deleterious effects of soluble amyloid beta species through mechanisms that are distinct from that of CT1812 yet potentially complementary. Some of these other efforts seek to block the formation of toxic protein aggregates or induce immune responses against specific epitopes found only in amyloid beta oligomers and protofibrils. Given the complexity of the disease, we are encouraged that these approaches are beginning to show real clinical promise.
These are exciting times for those working to find new treatments for progressive neurodegenerative diseases. Drug developers are beginning to see success in clinical trials that we hope will lead to the availability of effective therapies for patients. For the first time in decades, we can see a horizon where patients and caregivers have multiple distinct and complementary therapies that can be used to develop effective treatment regimens that provide patients with clinical benefit, symptom relief and quality of life.
Anthony O. Caggiano, MD, Ph.D. is the chief medical officer (CMO) of Cognition Therapeutics. Dr. Caggiano has broad experience in the development of new medicines for neurological conditions. During his 17 years at Acorda Therapeutics, the last four as senior vice president of research and development, Dr. Caggiano oversaw preclinical and clinical development programs in neurological conditions such as multiple sclerosis, stroke and spinal cord injury. In addition, he directed a large team responsible for all aspects of early development through a combination of internal research efforts and external research collaborations. He built relationships with thought leaders, developed clinical trial strategies and participated in licensing activities.